|
|
|
Relationship between Systemic Inflammations and Benign Prostatic Hyperplasia (BPH): a Propensity Score-matched Analysis |
| 을지병원 , 국립경찰병원¹ |
| 이준호, 박연원¹, 조인창¹, 김병훈¹, 최재덕, 조정만, 강정윤, 유탁근 |
<strong>Introduction</strong>: We conducted this study to evaluated the relationship between BPH and systemic inflammations.
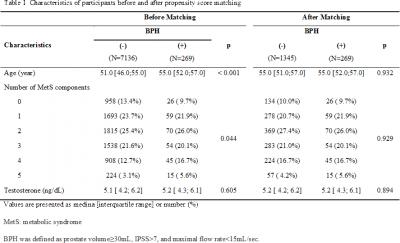
<strong>Methods</strong>: A total of 8727 males who had participated in a health checkup were analyzed. The IPSS, TRUS, uroflowmetry, testosterone, complete blood count, basic blood chemistry, and metabolic syndrome assessment were used for this study. BPH was defined as prostate volume≥30mL, IPSS>7, and maximal flow rate<15mL/sec. A propensity score matching was considered for 269 men with BPH (case) and 7136 men with no BPH (control), but ultimately, propensity scores were matched at a 5:1 ratio of controls to case group (1345 men in the control group and 269 men in case group).
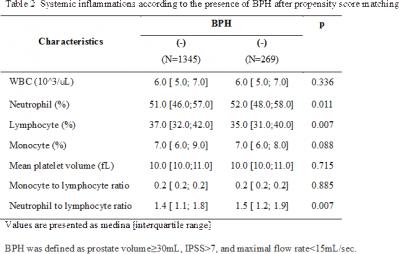
<strong>Results</strong>: After propensity score matching, age and number of metabolic syndrome component variables that were found to be significantly different before propensity score matching (table 1) were evenly dispersed and did not differ significantly between the groups (table 1). After matching (table 2), as an inflammatory marker, monocyte to lymphocyte ratio and mean platelet volume were not significantly different between two groups (table 2). However, neutrophil to lymphocyte ratio (a marker of subclinical inflammation) of the case group (BPH) was significantly higher than the control group (no BPH).
<strong>Conclusions</strong>: Among inflammatory markers, neutrophil to lymphocyte ratio was significantly correlated with the presence of BPH. Our data suggest BPH might be related to systemic inflammation.
|
  |
|
keywords : Systemic Inflammations, Benign Prostatic Hyperplasia, Testosterone |
|

