|
Cancer - Bladder, Pelvis, Ureter & Others(구연)
|
(E-047)
|
|
|
방광암 환자에서 로봇 보조 근치적 방광절제술 후 총 체내 요로전환술과 체외 요로전환술의 종양학적 결과 비교: 다기관 연구 |
| 연세의대 용인세브란스병원1, 연세의대 신촌세브란스병원2, 경북대학교병원3, 경희의료원4, 고려대학교 안암병원5, 부산대학교병원6, 인제대학교 부산백병원7, 성균관의대 삼성서울병원8, 서울대학교병원9, 분당서울대학교병원10, 가톨릭대학교 서울성모병원11, 한림대학교 강남성심병원12, 한림대학교 성심병원13, 한양대학교병원14 |
| 김종찬1, 나군호2, 한웅규2, 권태균3, 김태환3, 전승현4, 이상협4, 강석호5, 강성구5,남종길6,김완석7, 정병창8, 구자현9, 오종진10, 이상철10, 이지열11, 홍성후11, 이영구12, 이용성13, 박성열14, 윤영은14, 함원식2: Korean Robot Assisted Radical Cystectomy (KORARC) Study Group |
Purpose: This multi-institutional study aimed to compare oncologic outcomes of intracorporeal urinary diversion (ICUD) and extracorporeal urinary diversion (ECUD) following robot assisted radical cystectomy (RARC) in the patients diagnosed with bladder cancer.
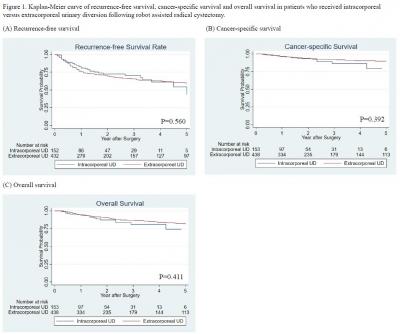
Materials and Methods: We retrospectively reviewed the medical records of 730 patients underwent RARC between April 2007 and May 2019 in 11 tertiary referral centers. We compared whether there is difference in the recurrence site between ICUD and ECUD group. Recurrence-free survival (RFS), cancer-specific survival (CSS) and overall survival (OS) were assessed using Kaplan-Meier methods between two groups. Cox regression model was used to identify the factors associated with RFS, CSS and OS.
Results: At a median follow up of 23 months, 199 patients experienced recurrence and 79 patients died (47 due to disease). Neobladder diversion was performed more frequently (70.8% vs 85.5%, p=0.001) and positive surgical margin observed more frequently (5.9% vs 2.1%, p=0.027) in ICUD group. Median follow up duration was shorter in ICUD group than ECUD group (16 months vs 26 months, p<0.001). Overall recurrence rate (36.5% vs 25.5%, p=0.013) and pelvic recurrence rate (12.1% vs 5.9%, p=0.031) were higher in ECUD group. However, there was no difference in 5-year RFS (43.2% vs 58.4%, p=0.516), CSS (79.3% vs 89.7%, p=0.392) and OS (74.3% vs 81.4%, p=0.411) between two groups. Multivariable analysis showed ECUD wasn’t associated with RFS (HR=0.982, p=0.920), CSS (HR=0.568, p=0.126) and OS (HR=0.642, p=0.124) compared to ICUD.
Conclusion: Although there was difference in recurrence rate between two groups, multivariable analysis showed diversion technique after RARC does not affect oncologic outcomes. Long-term follow-up is warranted to verify the oncologic outcomes between ICUD and ECUD group after RARC.
|
 |
|
keywords : Bladder cancer, Robot-assisted radical cystectomy, Urinary diversion |
|

